AI claims processing: Embrace AI to enhance claims management
Submitting a health or life insurance claim is often tedious for customers and underwriters alike. Collecting documents, filling forms, and waiting for decisions are frustrating, with lots of manual overhead and outdated document management systems. This represents significant inefficiency — Accenture estimates a whopping $160 billion productivity loss over five years across the global insurance industry.
The introduction of Artificial Intelligence (AI) into document processing is set to revolutionize this industry. AI claims processing integrates Machine Learning (ML), Optical Character Recognition (OCR), workflow automation, and data analytics to streamline the process, making it faster, more reliable, and more efficient.
This article explores how artificial intelligence can help you achieve end-to-end automation in the insurance claims process.
The mechanics of AI-driven claims processing
Traditionally, the claims process has been labor-intensive. It involves multiple steps: claim initiation, data entry, validation, decision-making, and payout.
Let’s say you have a car insurance claim. You'd have to provide myriad documents — accident reports, repair estimates, medical bills, if applicable, and so forth. These documents must be manually reviewed, verified, and approved, which takes time and resources.
AI claims processing replaces this tedious manual process with advanced technology to automate and streamline these tasks.
A video demonstrating how Nanonets can assist with claim processing.
Here's a simplified breakdown of how it works:
Step 1: Document ingestion
The AI system ingests the documents digitally, either through scanning physical documents or accepting digital files. This could include formats like PDFs, emails, and scanned images.
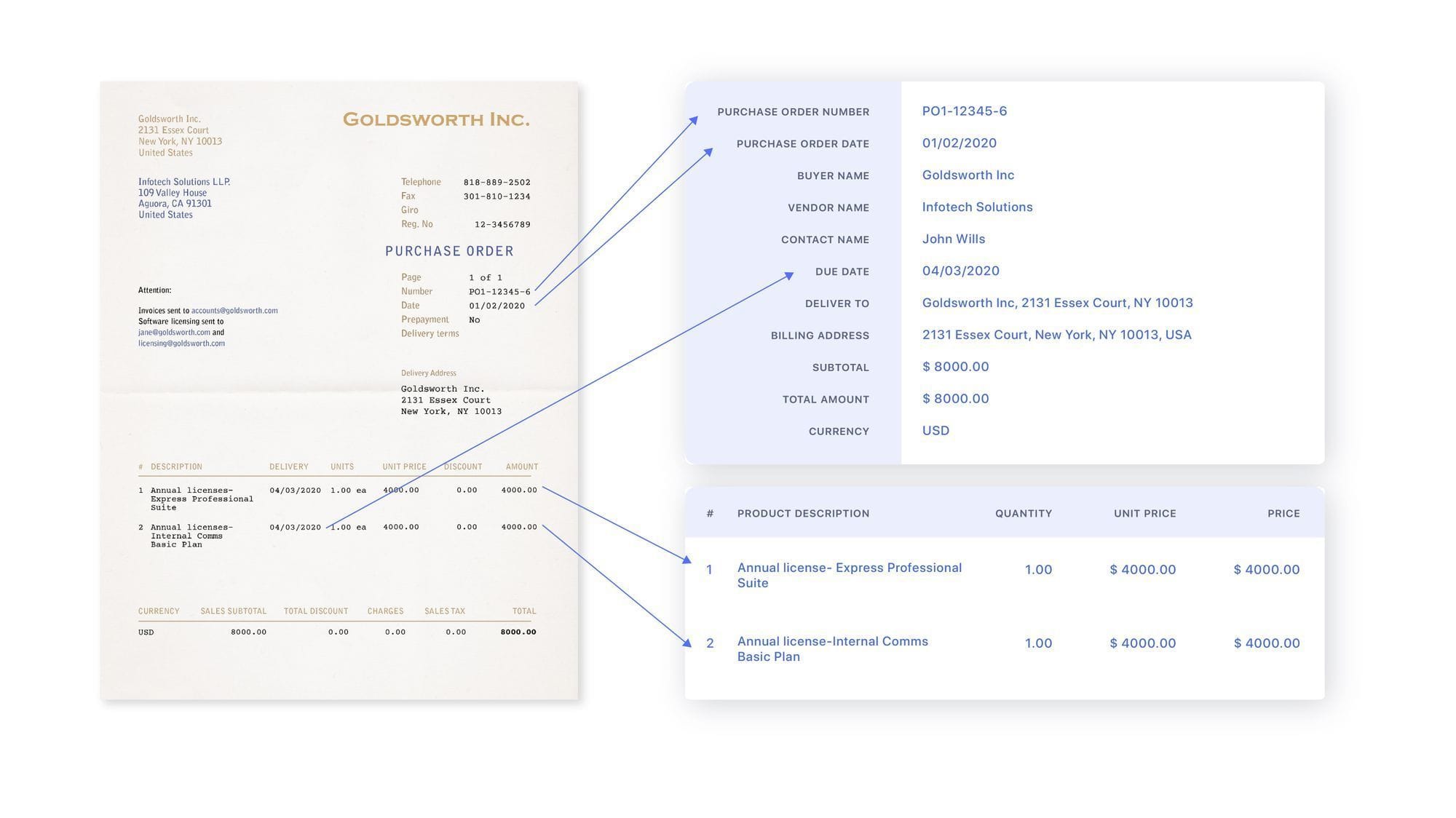
Step 2: Document understanding
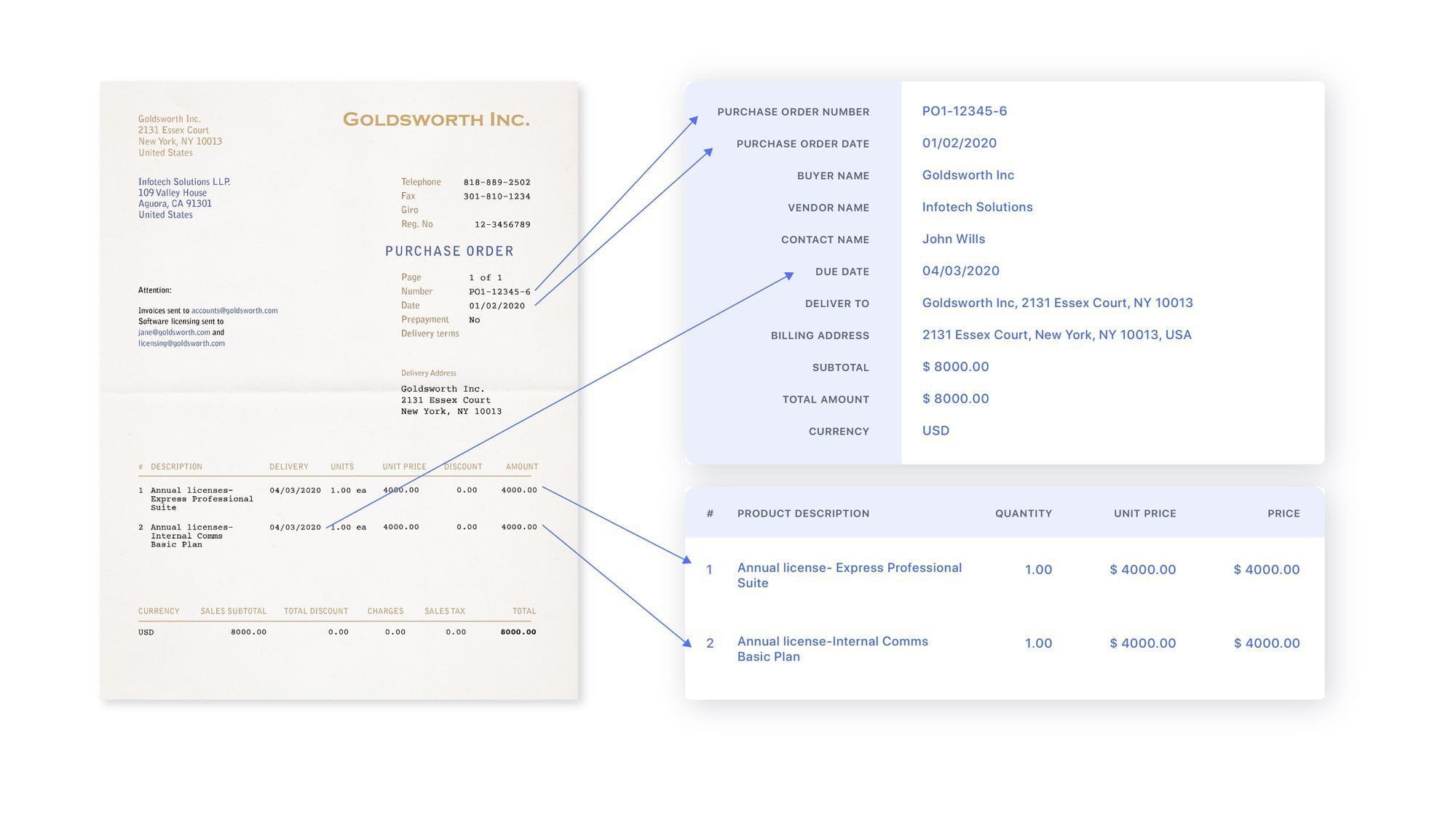
Next, the AI identifies and understands the information within the documents. It can extract key data points, like health insurance numbers, accident details, and costs, even from unstructured data.
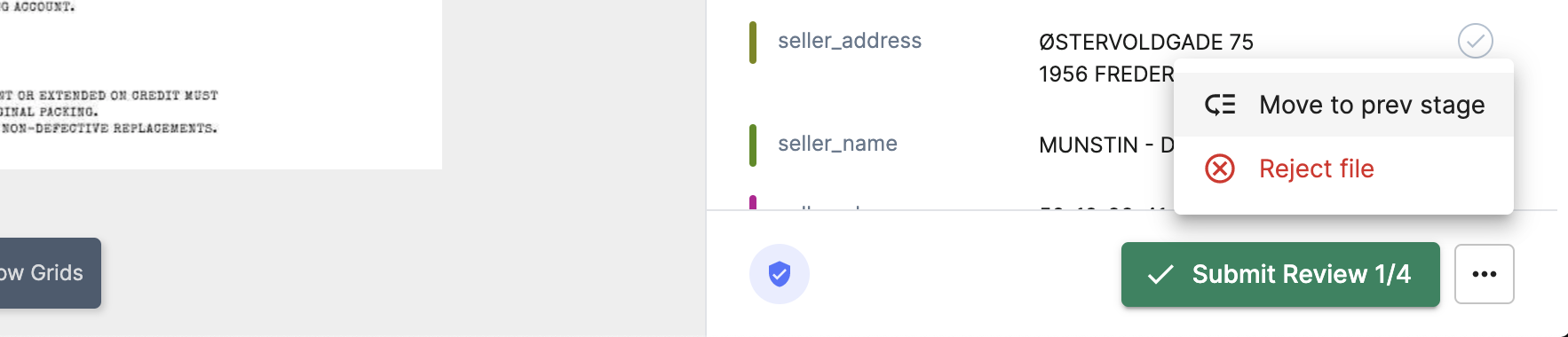
Step 3: Data validation
The system will then validate the extracted data against predefined rules and databases. This could include checking policy details, confirming accident details with third-party databases, and verifying cost estimates.
Step 4: Decision making
The AI system can then send the processed claim documents to the concerned department for final approval. It can also auto-approve claims based on specific criteria, significantly speeding up the process.
Step 5: Payout
Once approved, the processed files can be exported directly to the payment system to initiate the payout. The system can also notify the claimant of the final decision, providing transparency and improving customer satisfaction.
AI claim processing ROI calculator
Nanonets PRO plan cost = $499/month/model
- This ROI calculation is simplified, focusing solely on direct costs and excluding additional expenses such as staffing, supplies, storage, and potential claim processing delays.
- This calculation does not reflect The potential for increased revenue from reallocating employee time to higher-value tasks.
- Calculations are based on Nanonets' PRO plan, compared to the cost of employing a single clerk for manual processing.
- Consideration of larger ROI benefits from factors not included in this calculation is suggested.
- Nanonets offers a pay-as-you-go model suitable for smaller businesses or lower document volumes, with the first 500 pages free, followed by a charge of $0.3 per page.
- Depending on claim document volume and service scale, a full-time clerk may not be required to manage Nanonets.
Notes and assumptions

Move at light speed with accurate data extraction, faster approval cycles, and seamless data flow between your business systems.
Tips to streamline your claim processing workflow with AI
Claims processing workflows are ripe for automation with AI. By handling repetitive tasks like data extraction and document routing, AI systems allow insurance companies' staff to focus on higher-value claim assessment.
Here are a few tips to leverage AI capabilities and streamline your claims processing workflows for greater efficiency.
1. Enhance data accuracy with best-in-class OCR
Manual data entry is prone to errors and inaccuracies. While traditional OCR technologies can help, they often fall short when dealing with complex or unstructured documents.
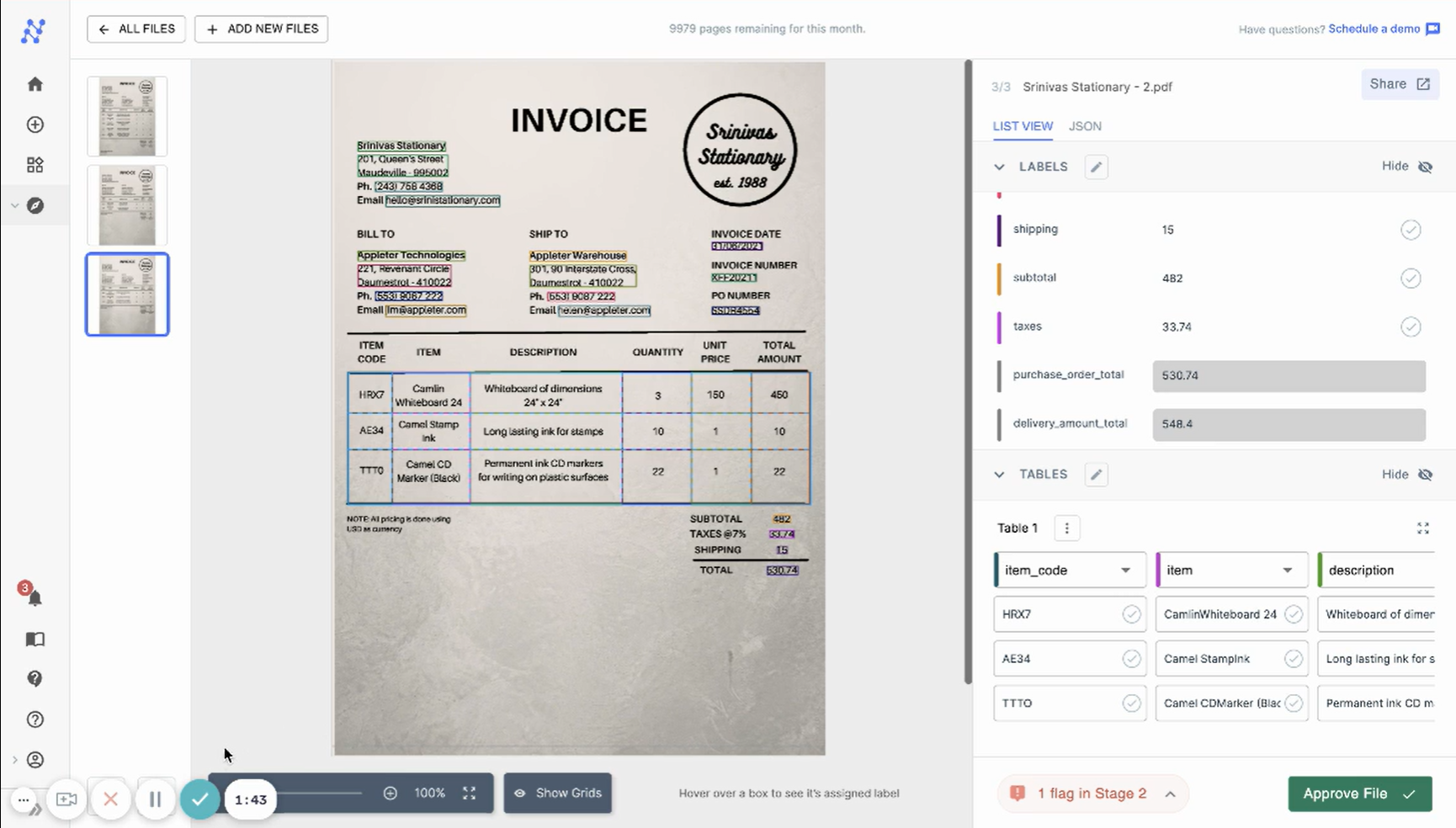
Nanonets' AI-powered OCR technology provides error-free data extraction capabilities, even from unstructured documents. It accurately captures and digitizes vital details from your documents, drastically reducing manual entry errors and saving significant processing time. Moreover, it overcomes language barriers, region-specific laws, and currency formats, making it a powerful tool in your claims-processing workflow.
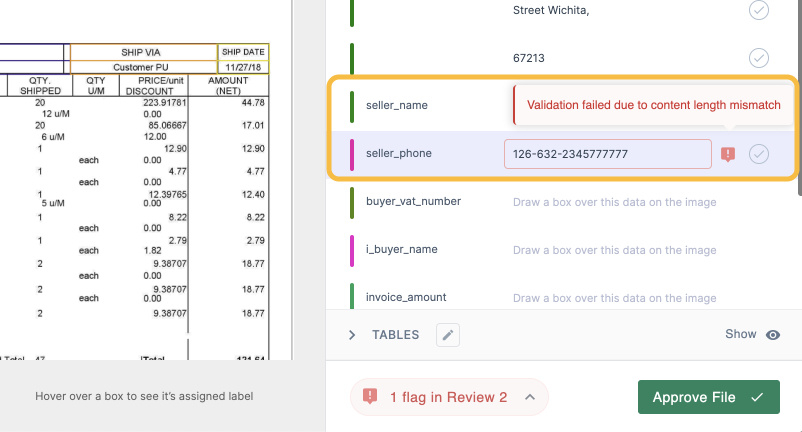
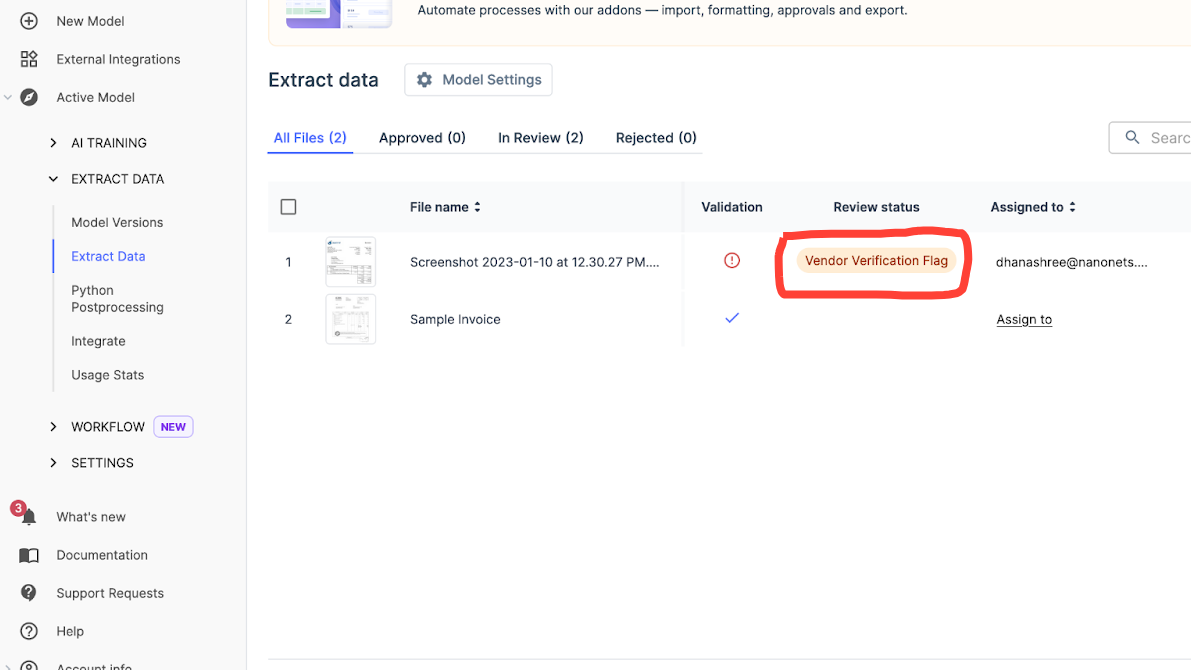
2. Enable real-time validation
Integrate rules-based validation of extracted claim data against databases of policies, claims history, etc. This instantly flags any discrepancies for review before claims move further, reducing fraud and errors.
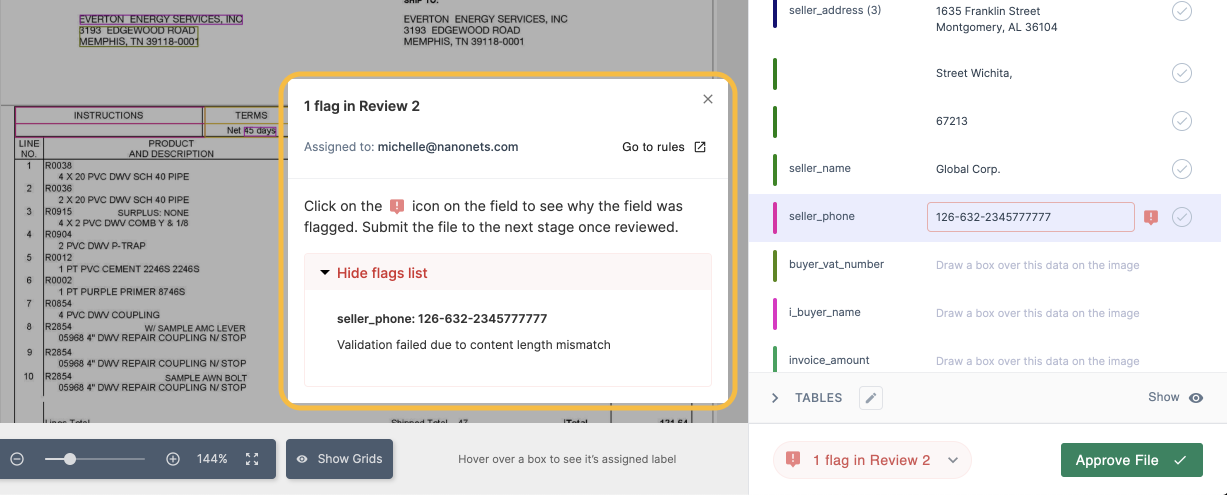
With Nanonets, you can effortlessly verify a claimant's policy number, personal details, and accident description against multiple databases. This automated process ensures that any discrepancies are flagged and sent for manual verification, providing you with accurate and reliable information every time.
2. Automate document routing
Create automated workflows to sort and classify incoming claims based on their nature, value ranges, policy categories, and other relevant factors. Afterward, these claims can be directed to the appropriate processing teams for timely and efficient handling.
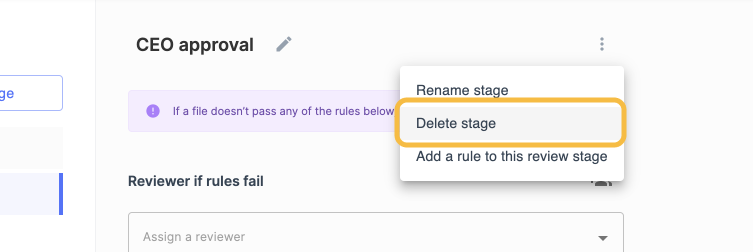
Nanonets can seamlessly capture and process crucial information from various sources, regardless of language or structure. Using its contextual understanding of documents, Nanonets efficiently categorizes and directs the data to the appropriate team, saving significant time and effort that would otherwise be spent manually sorting through it.
3. Trigger proactive alerts
Automatically notify stakeholders of claim progress via email, SMS, or in-app alerts to increase transparency and customer satisfaction.
Nanonets brings an end to the hassle of customers checking for updates on their claims by enabling you to send real-time alerts to claimants about the status of their claims, from under review to approval and even payout initiation. This adds convenience to their experience and enhances their overall satisfaction.
4. Ensure scalable processing
Cloud-based AI solutions can scale seamlessly to handle increasing claim loads without additional infrastructure. This saves costs with no in-house infrastructure upgrades needed for growth in claim volumes.
Nanonets offers pay-as-you-go pricing where you can quickly scale up or down based on your needs. Its cloud-based AI engine handles increasing claim volumes effortlessly, ensuring consistent performance regardless of the load.
5. Strengthen fraud detection
Enhance your fraud detection strategies with AI-powered predictive analytics. Implement rules to flag suspicious claims based on patterns identified from historical data.
With Nanonets, you can leverage AI to spot fraudulent patterns, flagging suspicious claims for further investigation. This helps you minimize losses due to fraud.
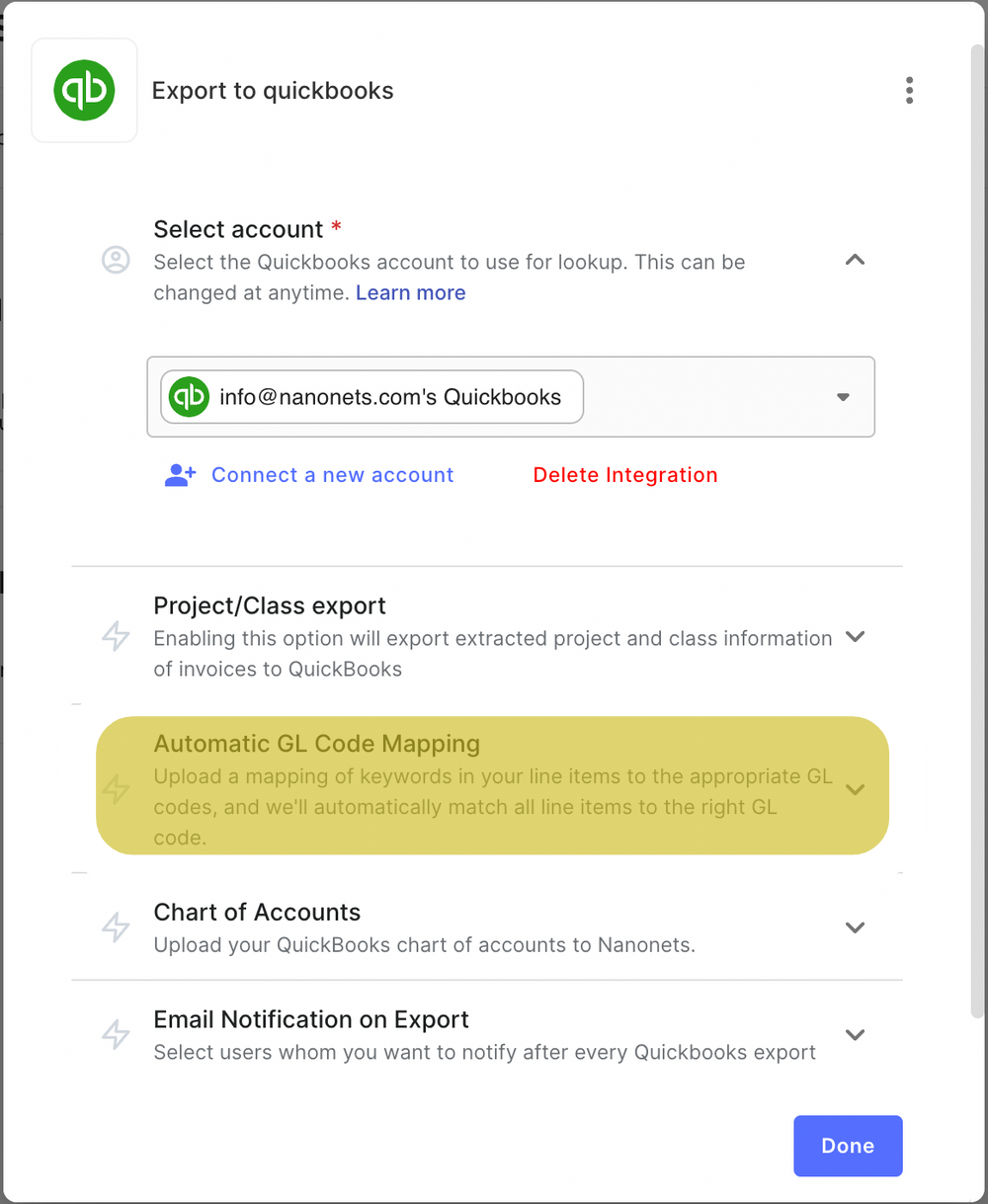
6. Ensure seamless data flow between systems
Let’s say you have a form on your website where customers can file claims. The submitted information should automatically flow into your claims processing system. If you are a Nanonets user, you can set up Zapier integration to import and extract data from your Webflow or Shopify forms directly into your Nanonets dashboard.
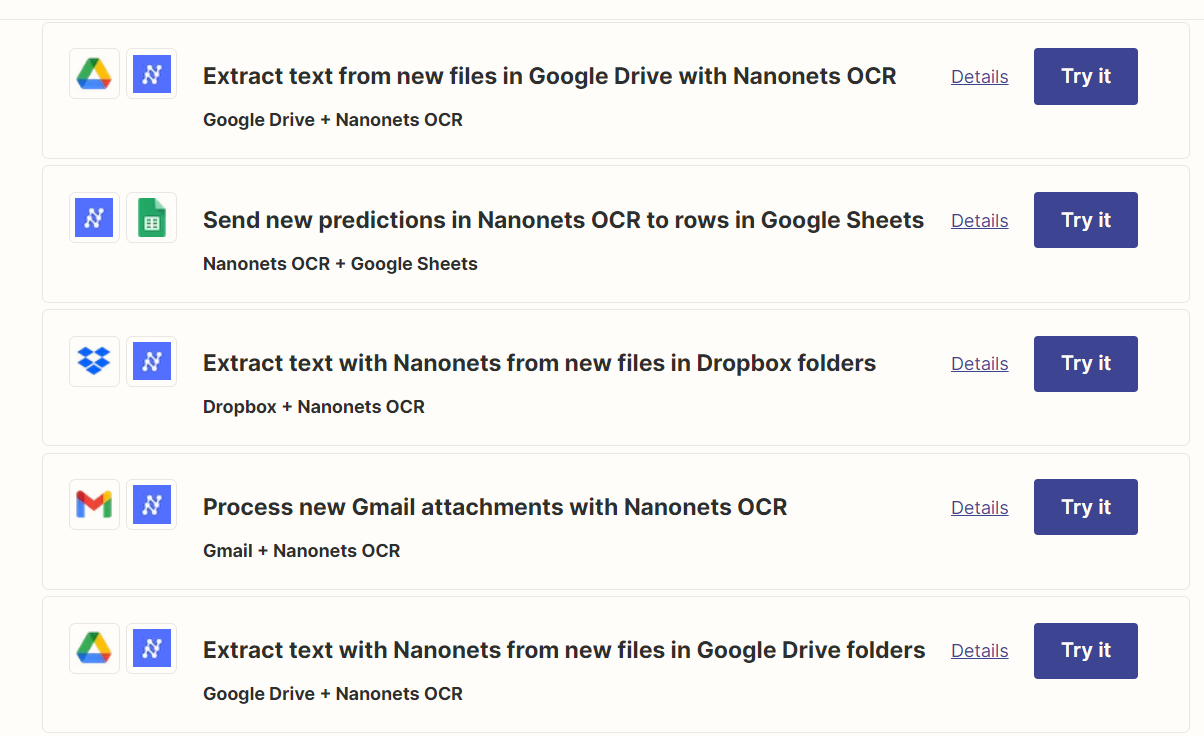
This seamless data flow eliminates manual data entry, accelerating processing times and reducing errors. Moreover, you’ll be able to act quicker on claims, creating a streamlined customer experience.
7. Implement data transformation for better data quality
Ingest data from documents and forms into standardized digital format for easy analysis. Clean noisy data, validate information, and enrich data with external sources.
With Nanonets, you can use our rule-based no-code workflows to automate data enhancement tasks such as date formatting, database lookup, data matching, and even removing commas or capitalizing data.

Final thoughts
Insurance companies can find it challenging to navigate the complex landscape of claim processing. Manual processes are time-consuming, prone to errors, and lack transparency and efficiency.
With Nanonets' AI-OCR capabilities, insurance companies can automate and streamline their claims process. Embrace the future of claim processing with Nanonets. Increase your processing speed, reduce costs, and deliver a superior customer experience.